TDRA Seed Fund Competition 2024
Description
The Toronto Dementia Research Alliance (TDRA) is pleased to announce a seed fund competition for 2024. These awards – valued at up to $70,000 – will be granted to collaborative projects that advance scientific knowledge in the field of dementia. There will be up to three seed funds available for projects that focus on neurodegenerative disease/dementia in general.
Objectives and Scope
- The project proposal need to focus on neurodegenerative disease/dementia
- These seed funds provide support for investigators during the critical period between the initiation of research and the receipt of sustained funding
- The funding will be for collaborative projects that bring together investigators across TDRA sites
- The more novel and innovative the project, the more competitive the application
Eligibility
Proposals will be deemed eligible based on the following:
- Principal Investigators must have a scientific appointment at one of the TDRA partner sites: University of Toronto, Baycrest, the Centre for Addiction and Mental Health, Ontario Shores Centre for Mental Health Sciences, Sunnybrook Health Sciences Centre, Unity Health Toronto, or the University Health Network
- Collaborative Projects: Two Principal Investigators (PIs) are required for projects to be considered collaborative; the PIs must be from two different TDRA sites, OR have a combination of pre-clinical and clinical research focus
- Previous award winners of the Temerty-Tanz-TDRA Seed Fund are not eligible to reapply as principal applicants
- Women and members of under-represented groups are strongly encouraged to apply
- Projects that focus on issues in traditionally underrepresented groups, such as Black, First Nations, Inuit, or Métis communities are strongly encouraged to be submitted
Apply
We are not accepting applications for the Seed Fund Awards at this time.
Meet the 2024 Seed Fund Awardees
Does CPAP improve cognition in vascular cognitive impairment and Alzheimer's disease?
Principal Applicants: Mark Boulos (Sunnybrook), Paul Verhoeff (Baycrest)
Obstructive sleep apnea (OSA) is common in people with vascular cognitive impairment (VCI) and Alzheimer's disease (AD), and can make cognitive problems worse. Previous studies suggest that treating OSA with continuous positive airway pressure (CPAP) may help improve attention and executive function. However, these studies have had limitations, such as small sample sizes and inconsistent follow-up.
The study team is currently conducting a study comparing two methods for diagnosing OSA in patients with cognitive impairment: in-laboratory polysomnography (iPSG) and home sleep apnea testing (HSAT). With the TDRA Seed Fund, the project will expand to include a sub-study that will track cognitive changes in patients using CPAP after six months. This sub-study will help determine if treating OSA with CPAP can improve cognitive outcomes in patients with VCI/AD. It will also explore whether CPAP affects sleep quality, mood, daily functioning, and caregiver burden—key factors that impact quality of life.
Digital phenotyping of circadian rhythm using location data in long-term care
Principal Applicants: Andrea Iaboni (UHN), Andrew Lim (Sunnybrook)
Changes in sleep and daily activity patterns, such as excessive daytime sleepiness or “sundowning” (increased agitation and confusion in the evening), are common in dementia and can significantly impact both quality of life and caregiver burden. In long-term care (LTC) settings, disrupted sleep can hinder residents' participation in activities, and compromise their safety by increasing the risk of falls or the use of sedative medications.
This study will use data from existing safety systems in LTC homes to monitor for circadian rhythm disruptions and improve diagnosis and care. These safety systems track residents' movements with real-time location technology, which gathers valuable information about residents’ rest and activity patterns. The study team has shown this data is effective for tracking rest-activity rhythms in people living with dementia. The next step is to analyze these patterns in a larger group of LTC residents over the course of a year, using machine learning to identify common disruptions, and leveraging this data to enhance care and sleep management strategies moving forward.
Prefrontal cortical plasticity in mild cognitive impairment: Implications for eye movement and language processing
Principal Applicants: Hamed Azami (CAMH), Jennifer Ryan (Baycrest)
Alzheimer’s Disease (AD) and Mild Cognitive Impairment (MCI) can affect eye movement and language processing, both of which are controlled by the Dorsolateral Prefrontal Cortex (DLPFC)—a part of the brain involved in higher-level functions like memory, attention, and decision-making. This study will explore how changes in the DLPFC impact these abilities in older adults.
Researchers will use two types of tasks: a "preferential viewing task" to assess eye movements and memory, and language tasks to evaluate language processing, while recording brain activity using Electroencephalography (EEG). In the preferential viewing task, participants will look at images of familiar and new items. Normally, people spend more time looking at new items because their brain recognizes them as unfamiliar. In people with MCI, this ability may be weaker. Eye movements and brain activity, particularly theta waves—which are brain signals linked to memory and attention—will be measured. For language tasks, participants will practice understanding and producing sentences, while beta waves, which are important for language processing, are recorded. The study will compare how well older adults with MCI perform these tasks against healthy adults. The goal is to identify brain activity patterns to better detect and track eye movement, memory, and language issues in MCI, ultimately improving early diagnosis of conditions like Alzheimer's.
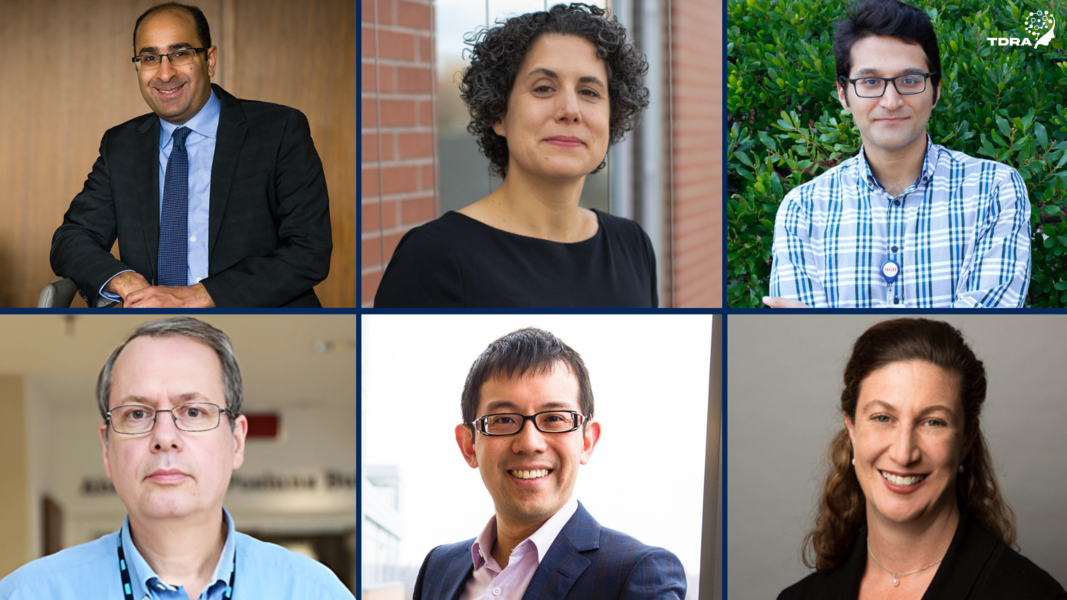
Pictured left to right: Mark Boulos, Andrea Iaboni, Hamed Azami (top row), Paul Verhoeff, Andrew Lim, Jennifer Ryan (bottom row)