Reducing Dementia Risk in Type 2 Diabetes
Spotlight on: Dr. Walter Swardfager

Our brains require fully half of all the sugar energy in the body to function properly. If blood sugar levels rise or fall outside of normal range, this can throw the brain off balance, potentially predisposing us to dementia.
Understanding the connection between type 2 diabetes and dementia may be a critical step in developing better treatments for both conditions.
Diabetes is a chronic disease that affects how our bodies turn food into energy. Much of the food we eat is converted by the body into sugar (glucose), and released into the bloodstream. When our blood sugar goes up, it signals our pancreas to release insulin, which moves the glucose from the blood stream into the cells, for use as energy.
With type 2 diabetes, our body can’t use insulin as well as it should, which results in too much sugar in the blood. Other factors such as hormones and fats come into play as insulin resistance develops. Over time, diabetes can cause nerve and blood vessel damage which affects our heart, eyes, kidneys, feet, and hands, and it can also affect our brain.
The impacts of diabetes on the brain can result in problems with memory and information processing, mood shifts, and over time, a predisposition to develop Alzheimer’s disease or vascular dementia.
It is helpful for people living with diabetes to keep their blood sugar within target levels to minimize harmful impacts on the body and brain. In that sense, diabetes is considered a modifiable risk factor for dementia; however, sugar levels do not fully explain the risk, necessitating further study.
TDRA’s Dr. Walter Swardfager studies the contributions of metabolic disease (of which diabetes is a primary example) to cognitive decline and dementia, and has added significantly to this field. Dr. Swardfager is an Associate Professor in the Department of Pharmacology & Toxicology at the Temerty Faculty of Medicine, University of Toronto, a Scientist at Sunnybrook Research Institute, and the Canada Research Chair in the Clinical Pharmacology of Cognitive Neurovascular Disorders.
Dr. Swardfager is Principal Investigator of The Sunnybrook Type 2 Diabetes Study (S2DS), a collaborative study involving dozens of investigators with complimentary areas of expertise. It is conducted in collaboration with the UHN Toronto Rehabilitation Institute Cardiac Rehabilitation Program, with another TDRA investigator Dr. Paul Oh as on-site lead. The study infographic is shown below.
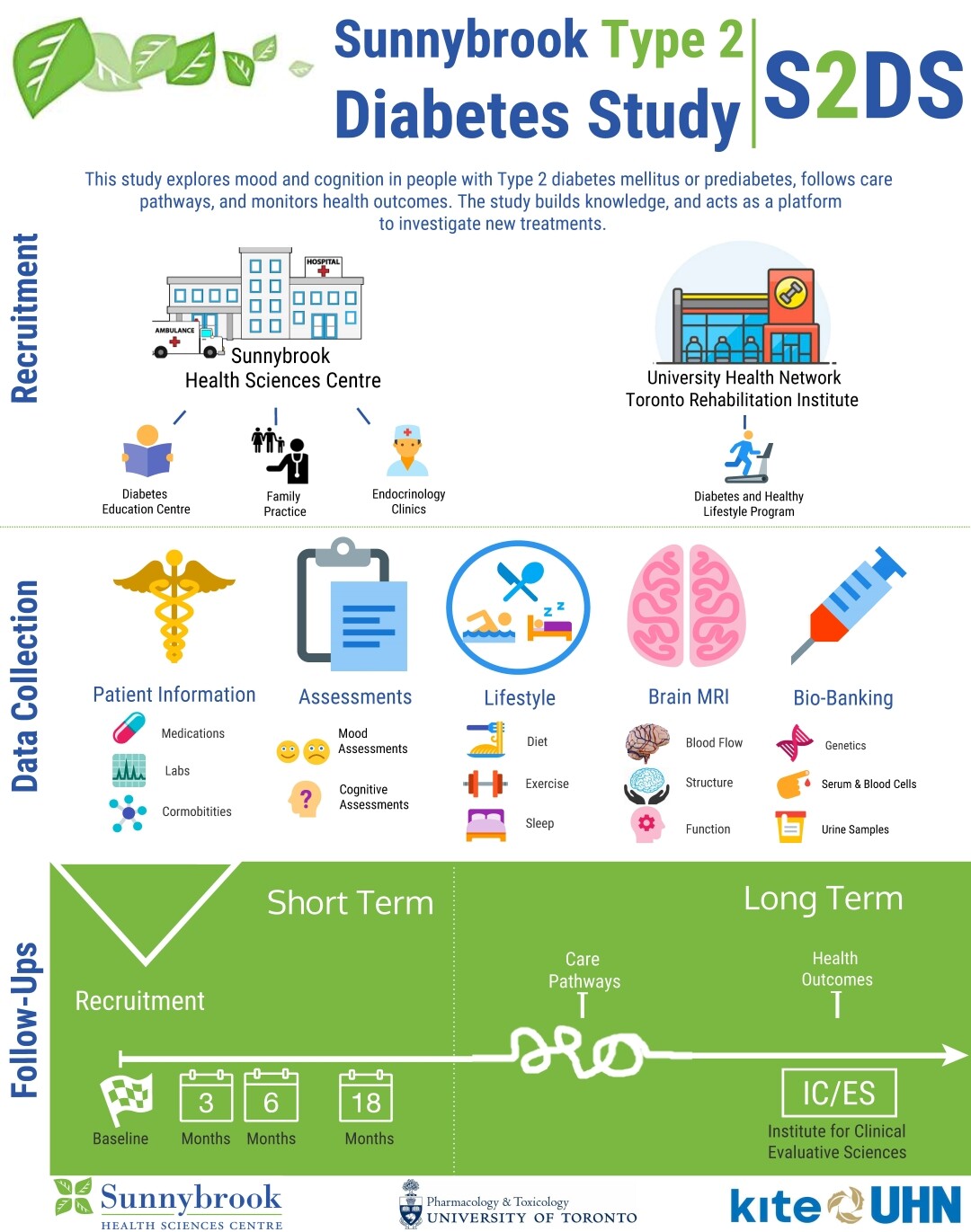
The S2DS is an observational study of people living with type 2 diabetes or “prediabetes”, its pre-symptomatic stage. It aims to understand the causes, manifestations, and clinical consequences of mood and cognitive complications. Participants recruited from Sunnybrook are receiving care from services there, while participants recruited from the Toronto Rehab are undertaking a 4-month stepped hybrid (home and clinic based) aerobic plus resistance exercise intervention.
Study assessments are conducted at baseline, 3 months, 6 months and 18 months. The main factors studied include:
- cognitive performance - assessed using a detailed set of neurocognitive tests
- mood symptoms - assessed via research criteria for a depressive episode and self-report instruments, and
- Other lifestyle factors, including physical activity, sleep quality, diet, and subjective stress
Diabetes complications and characteristics are monitored, as are all medications and supplements used. With permission, participant data are linked to public health records to uncover long-term outcomes and health services utilization.
“The study provides a 360 on the brain in type 2 diabetes. We can see small changes over 18 months, and potentially more significant changes, like progression to a dementia diagnosis, in the longer term. We hope to develop new strategies to improve diabetes care and prevent dementia at the same time.” says Dr. Swardfager.