Dementia Risk Factors: Connecting Sleep Disorders, Obesity and Hypertension
Scientist Explains with Dr. Michael Mak
March 17, 2024
Why is sleep so important?
We spend a third of our lives sleeping. Many processes that affect our overall health occur while we sleep. It is the time when our body repairs and recuperates, and our immune system is able to get stronger. In fact, it is believed that the waste products of our brain are shuttled away during sleep, removing potentially harmful toxins that build up throughout the day.
Sleep quality is therefore a critical factor for cognitive health and dementia.
Introduction to Sleep Medicine
While sleep is a critical aspect of our overall health, it has been taken for granted and under-explored. Freud famously interpreted dreams as a way to explain the cause of mental illness. Sleep medicine as a field was perhaps born in the 1950s when REM sleep was discovered. Since then, many tests and treatments for sleep problems have been developed. We now know that sleep is crucial to almost all forms of life and their survival.
Sleep medicine is a broad, multidisciplinary field that covers a large number of disorders that impede the therapeutic, quality sleep the body needs. Many patients in sleep clinics have sleep apnea (where breathing is interrupted throughout the night, depriving the body - including the brain - of oxygen), insomnia (problems falling or staying asleep), narcolepsy (extreme sleepiness), and/or many other conditions.
While sleep doctors see patients in many age groups, sleep disorders (for example, insomnia and sleep apnea) disproportionately affect older adults; therefore, sleep clinics may serve more elderly patients than other groups.
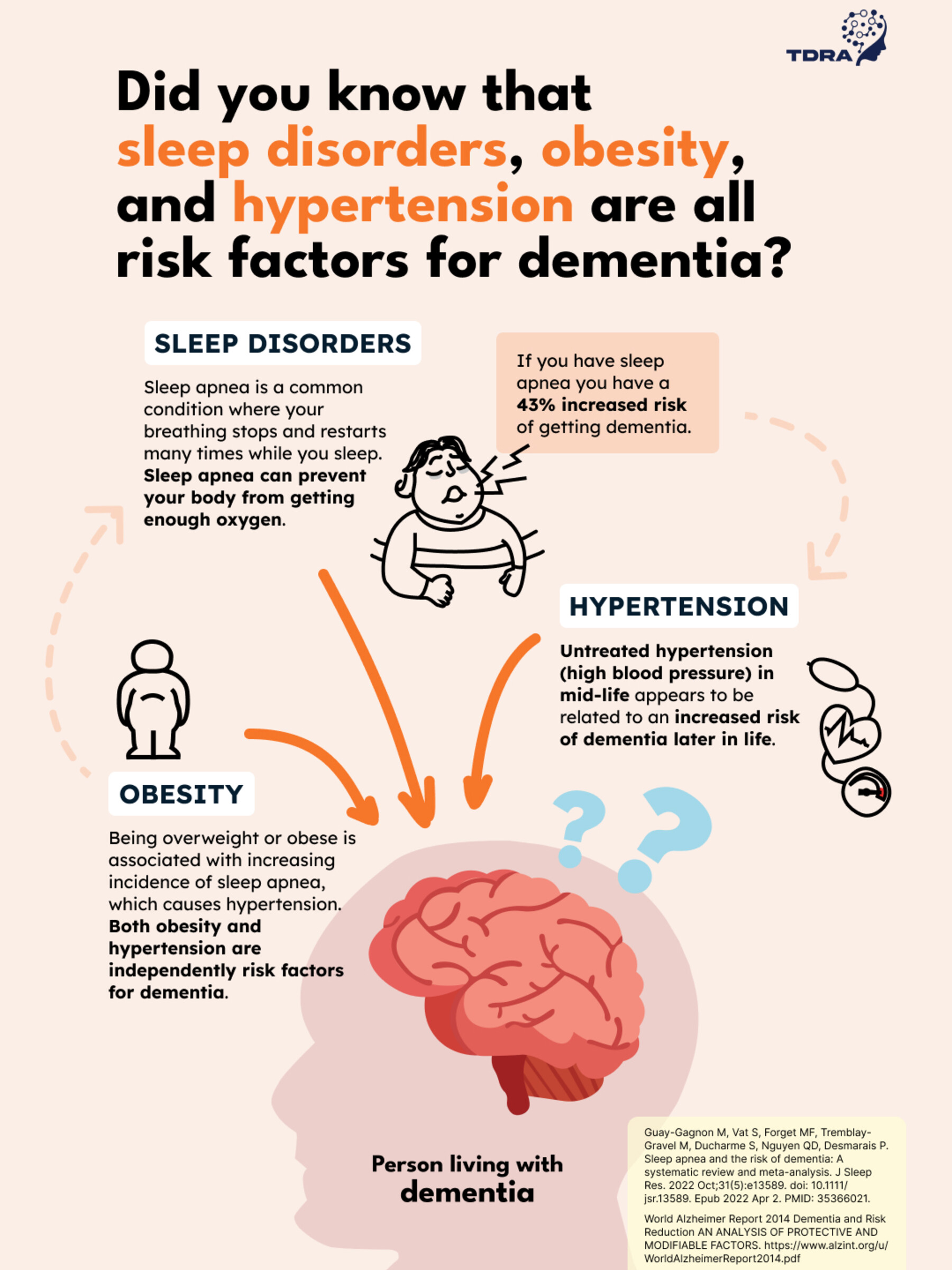
Inter-related dementia risk factors
Many factors having to do with physical and mental health can affect our quality of sleep and these are often inter-related. A person living with obesity has a heightened risk of having sleep apnea, due to their airways being more crowded. This makes it far easier for the airways to close up inappropriately during sleep, leading to the release of ‘fight or flight’ hormones, which cause high blood pressure. Sleep apnea also reduces the amount of time a person spends in deep sleep, which has been linked to problems with memory and possibly, the development of dementia. Finally, a person living with untreated sleep apnea may have higher levels of sleepiness that makes it harder for them to exercise, which may lead to weight gain.
This circular relationship between sleep apnea, high blood pressure and obesity - all independent risk factors for dementia - is depicted below.
Sleep Medicine protocol with Dr. Michael Mak
Dr. Michael Mak is a psychiatrist and sleep medicine specialist at the Centre for Addiction and Mental Health in Toronto. He is also the Vice President, Clinical, of the Canadian Sleep Society. Dr. Mak sees many patients who have, or are at risk for dementia, in his clinical work. He takes a holistic approach that incorporates all their health indicators when treating his patients.
Patients are first seen in clinic to discuss symptoms; and if indicated, they undergo testing for sleep disorders at the sleep laboratory. When conditions like sleep apnea are treated in Dr. Mak’s practice, through CPAP therapy or other methods, there is chance that their risk of dementia can be reduced, or its progression slowed down. Treatment of sleep apnea can also improve blood pressure, which may reduce dementia risk as well. Lastly, patients are encouraged to lose weight if they have obesity, as we know that regular exercise may reduce dementia risk, and has a positive effect sleep apnea and hypertension (high blood pressure).